WASHINGTON – Reaching out to uninsured minorities and getting them to enroll in insurance programs is a key concern for health officials trying to implement the new health care law.
At a Department of Health and Human Services minority health advisory committee meeting on Tuesday, members questioned the government’s ability to reach the uninsured, especially minorities, based on current Medicaid expansion plans.
A major tenet of the Affordable Care Act creates a minimum Medicaid income eligibility level nationwide. The federal government will fully fund the costs of the newly eligible Medicaid recipients for three years, and then phase down the support to 90 percent by 2020, with states making up the difference.
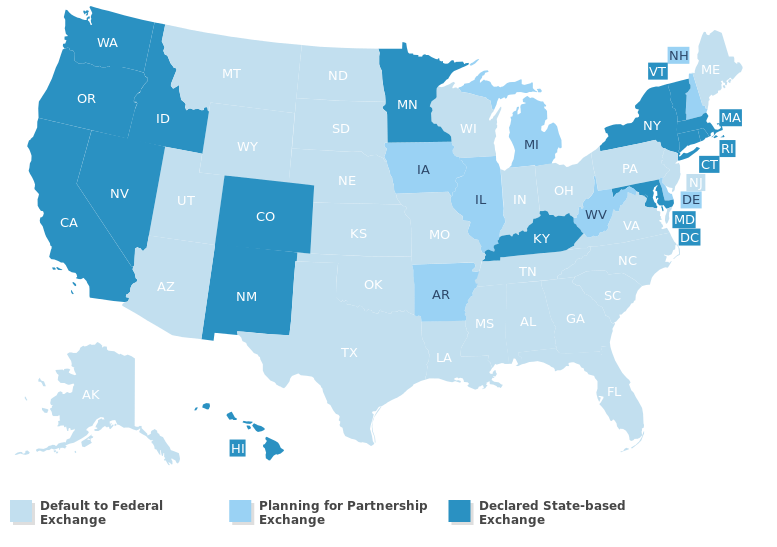
Twenty-one states do not plan on broadening
Medicaid programs, with another six still weighing their options.
Source: Kaiser Family Foundation
Twenty-one states do not plan on broadening Medicaid programs, with another six still weighing their options.
According to a Kaiser Family Foundation study, nearly half of uninsured people of color reside in states not moving forward with Medicaid expansion. This also affects many immigrants who will remain ineligible for coverage.
Edward Martinez, a member of the advisory committee and a representative of the National Association of Public Hospitals and Health Systems, said the states opting out tends to be those with high numbers of minorities, concentrated in the South.
“At least geographically it shows that we have a separate but unequal health care system,” Martinez said.
The issues of targeting minority groups is complicated by differences in state-based Medicaid programs.
“Coverage expansions offer an important opportunity to significantly reduce disparities in coverage,” said Jessica Stephens, a policy analyst at the Kaiser Family Foundation who addressed the committee. “But there will be coverage gaps in part because of some states choosing not to expand Medicaid.”
Committee members additionally expressed concern over the ability of current marketing and educational approaches planned to publicize the new eligibility to reach minority groups.
“We are targeting our programs in high concentration areas where the most vulnerable and most uninsured are,” responded Kelly Dinicolo, a technical advisor at the Center for Medicare & Medicaid Services.
Programs in place include informational websites in English and Spanish, a call center with language translations, and enrollment assistance through web applications and in-person help.
The Kaiser Family Foundation provided guidance for creating informational programs based on previous Medicaid experience:
- Combination of broad and targeted outreach strategies
- Accessible, welcoming, and simple application and enrollment
- One-on-one enrollment assistance from trusted individuals
- Facilitating renewals of coverage
Stephens noted that in-person assistance was one of the most important outreach methods.
“Not only does that help people enroll, it helps people use coverage more effectively once they get enrolled because they had information,” Stephens said. “It’s not just important to have coverage but to make sure that that coverage is continued and renewed.”
Dinicolo said CMMS will have one-on-one programs in place in September, just one month before the Oct. 1 marketplace launch date.
The Congressional Budget Office estimates that the Affordable Care Act will extend coverage to 33 million Americans who would otherwise be uninsured.
