WASHINGTON – Amid a worker shortage exacerbated by the pandemic, health care professionals suggested to senators Thursday that Congress boost opportunities for their industry and reduce regulations.
“I have heard from so many nurses and doctors and other health care workers back in Washington state about how hard this pandemic has been,” Sen. Patty Murray of Washington said. “Health care workers have handled long hours, overcrowded facilities, fighting a deadly new virus, often while receiving low pay … They’ve seen the pain of this pandemic up close and personal, and it’s taken a real toll.”
Washington Gov. Jay Inslee activated about 100 members of the National Guard in January to assist hospitals facing staffing shortages, while Idaho Gov. Brad Little sent 75 members of the National Guard in February to help Primary Health Medical Group and the Idaho Department of Correction. More than 500 additional workers were contracted to work at Idaho hospitals overwhelmed by COVID-19.
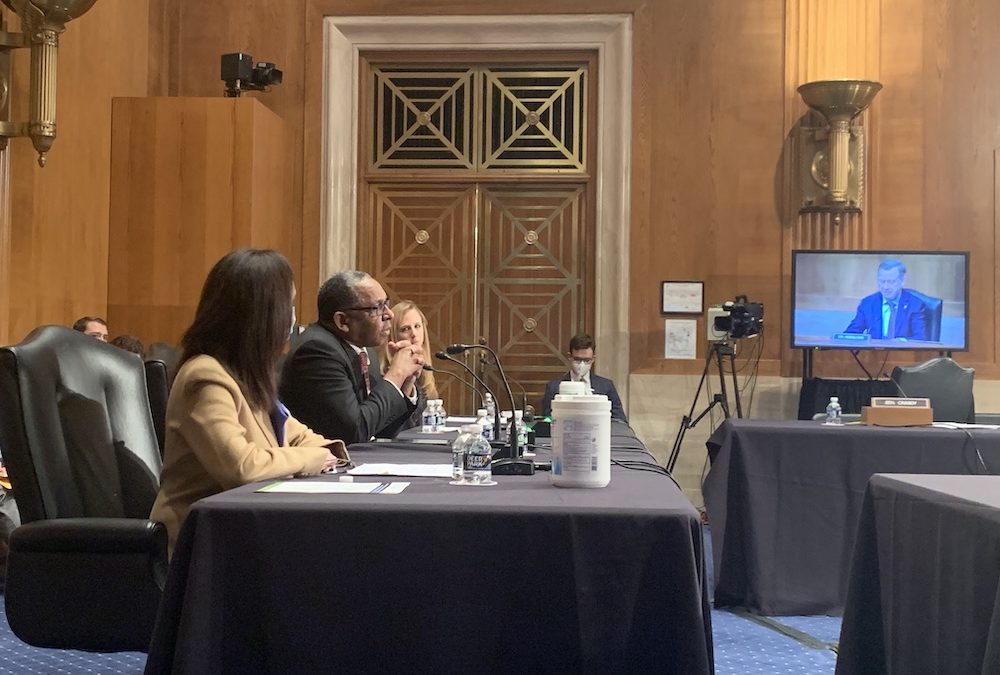
Murray, who serves as the chair of the Senate Health, Education, Labor and Pensions committee, joined other members of the Subcommittee on Employment and Workplace Safety Thursday to discuss solutions to the health care workforce shortage.
The United States could face a shortage of up to 124,000 physicians by 2034, according to data released by the Association of American Medical Colleges in June.
“After all they have done for our communities, we owe it to our health care workers and everyone on the front lines of this pandemic to listen to their experiences and respond to the challenges they are dealing with,” Murray said.
Nurse practitioners could help alleviate the health care worker shortage by serving as primary care providers, said Margaret Flinter, a nurse practitioner and the senior vice president and clinical director of Community Health Center Inc. in Middletown, Connecticut.
“Where is the next generation of primary care providers going to come from?” Flinter said. “I answer: It’s already here. Nurse practitioners are here in number and in their focus on primary care.”
In order to prepare nurse practitioners to serve as primary care providers, Flinter said they should have the opportunity for post-graduate residency or fellowship training similar to that offered in medicine and dentistry. Since 2007, Flinter has led efforts to develop these types of nurse practitioner residency programs.
When there is a gap between preparation and actual practice, Flinter noted this can lead to burnout, frustration and the departure of nurse practitioners from primary care roles and the practices that need them.
Norma Quinones, the nursing services manager at Clinica Family Health, said the National Institute for Medical Assistant Advancement, could provide another model for addressing the shortage. The institute, which trains medical assistants, creates an accessible entry point for long-term health care careers and helps diversify the U.S. workforce, Quinones said.
The institute allows students to work part time during the program, providing opportunities for nontraditional students, such as single parents, recent immigrants, first-generation high school graduates and those who enter the health care workforce at an older age.
For Reynold Verret, president of the historically Black Xavier University, it is essential to build pathways for a more diverse group of students to become health care professionals. Verret emphasized that these efforts need to begin with students in elementary and high school.
Rachel Greszler, a research fellow at the Institute for Economic Freedom and Opportunity at the conservative Heritage Foundation, said the shortage is also the result of regulatory burdens, particularly at the state level.
Greszler said states should eliminate unnecessary licensure and scope of practice laws that limit the health care workforce.
“Doctors and nurses should be able to practice their professions where the need is greatest and not simply within the geographic confines of their license,” Greszler said. “It’s particularly ludicrous when a provider can’t have a telehealth visit with a regular patient simply because they are out of the state at the time.”
Subcommittee chair John Hickenlooper, D-Colo., said the government needs to address these shortages now if it is to make a dent in the daunting shortages predicted for the future.
“The critical needs of the health care workforce were here before and will extend well beyond COVID unless we act,” Hickenlooper said.