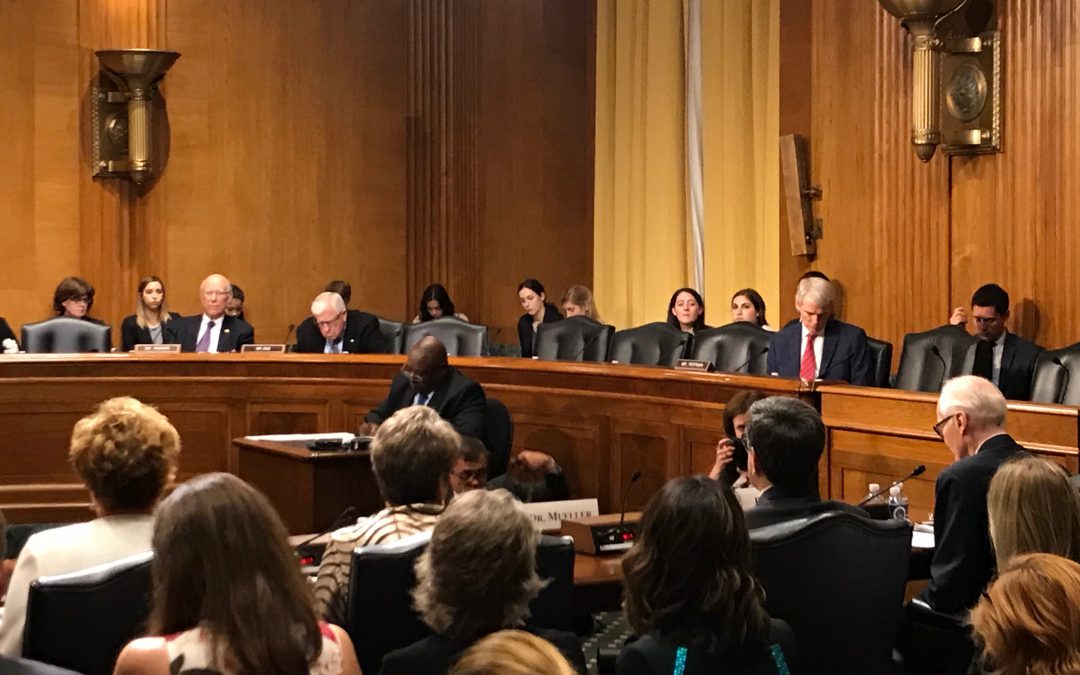
WASHINGTON — A financial crisis at rural hospitals driven by inadequate government funding is hurting millions of Americans’ access to quality healthcare, experts told the Senate Committee on Finance on Thursday.
Because rural communities have more senior citizens and disproportionately high rates of chronic illness and obesity, many people in those areas rely on Medicare and Medicaid, according to the Centers for Disease Control and Prevention. But reimbursements from the two federal programs to rural healthcare providers don’t always cover the cost of treatment, forcing hospitals and clinics to close, experts said.
“Given the financial pressure under their current…reimbursement structure, rural hospitals are frequently unable to address the health of their communities,” said Karen Murphy, chief innovation officer at Steele Institute for Healthcare Innovation at Geisinger.
Formerly the Pennsylvania Secretary of Health, she said she was “struck by the instability” of the rural hospitals in the state.
Murphy now advocates for a new financial model in which rural hospitals are paid monthly from a “global budget” based on the hospital’s annual revenue. Under this plan, hospitals can tailor their services to community needs, she said, and would still treat patients with Medicare, Medicaid and private insurance.
“This approach is expected to provide hospitals with a predictable revenue stream,” Murphy said.
Maryland first used the model and Pennsylvania is beginning to implement a global budgeting system as well.
Sen. Ron Wyden, the committee’s top Democrat, said the bipartisan budget deal signed by President Donald Trump in February extended an “important” program that funds “Medicare-dependent hospitals” — small hospitals in which more than 60 percent of the patients’ insurance coverage is through Medicare.
“That at least gives us some measure of predictability for the next five years, but it seems to me we’ve really got some heavy lifting to do,” the senator from Oregon said.
Since 2010, 83 rural hospitals have closed nationwide and hundreds more are at risk of closing, he added.
Wyden also warned of the Trump administration’s attempts to “slash” Medicaid funding, which he said would “turn rural America into a sacrifice zone where hospitals shut down and people cannot get the care they need.”
Committee Chairman Sen. Orrin Hatch, R-Utah, rebuked Wyden, saying rural hospitals had financial problems long before Trump became president.
“We can’t just spend more money on Medicaid and expect to solve every problem,” Hatch said.
Sen. Chuck Grassley, R-Iowa, plugged a bill he introduced last May. It would create a new Medicare classification allowing small, rural hospitals to choose to provide only emergency services, lowering their overall costs. Those hospitals would get reimbursements for the cost of transferring patients needing inpatient care. The proposal has co-sponsors from both parties and support from the American Hospital Association.
Konnie Martin, the CEO of San Luis Valley Health in Colorado, which includes two small hospitals and five rural clinics, also supported Grassley’s plan.
“Nearly 70 percent of our patients are covered by Medicare or Medicaid,” she said. “We constantly struggle to remain financially viable.”
Wyden, who said the hearing would inform town halls he plans to host in Oregon next week, spoke directly to Martin after her testimony.
“I’m going to remember what you said — ‘where you live should not determine if you live.’ That really sums up the challenge.”